The physiology of healthy skin: moisturisation, hygiene, care, advice
26 February 2015, by VERSCHOORE M. & SAINT LEGER D.
Summary
1 - PHYSIOLOGY OF HUMAN SKIN
1.1 - EPIDERMIS
This thin epithelial tissue (approx. 50-70μm) is in constantly renewal. It is composed of 4 major cell types :
– keratinocytes (approximately 95% of the cells), the constant renewal and transformation of which (keratinisation) from the stratum basale up to the skin surface, leads to the formation of this tissue the signature biochemistry of which is its high content in insoluble proteins, the keratins;
– melanocytes (approximately 3%), cells which produce the melanin pigments (eumelanin, pheomelanin), each melanocyte transferring these pigments (melanosomes) to about thirty surrounding keratinocytes, in the form of compact or diffuse granules;
– Langerhans cells (approximately 2%), which originate outside the skin (bone marrow) are the guardian immune cells which detect foreign and/or allergenic substances. Indeed they can circulate and ultimately alert the T-lymphocytes in the lymph nodes, presenting the « foreign » molecular structure thus provoking their specific multiplication and movement towards the sites of the invasion;
– Merkel cells (approximately 0.5%) which ensure the perception and conduction of various nervous impulses transmitted by as many as 2 million receptors distributed all over the skin. The epidermis becomes an aerial and a transmitter.
From a metabolic and energetic point of view, in contrast to a widely held belief, the skin (the epidermis) does not breathe. The epidermis functions mainly anaerobically, i.e. not metabolising sugars to their ultimate end (producing lactic acid instead of CO2 and H2O). Table I summarises some of the principal effectors to which the various epidermal cell types are sensitive.
Keratinisation, water and the epidermis
The healthy epidermis exhibits a low but constant rate of cell division: indeed the mitotic index of the stratum basale is in the order of 10% (percentage of cells dividing at a given time t). This fact is important because it indicates that the epidermis thus possesses a large reservoir of keratinocyte multiplications in case of need related to inflammatory and/or reparative processes (cuts, burns…). In cases of Psoriasis, a typical inflammatory disorder, the mitotic index approaches 100%.
The maturation process « keratinisation » or terminal differentiation, lasts 4 to 5 weeks ultimately ending in desquamation. Under normal conditions this phase ends in the release of terminal cells (corneocytes) in the form of an isolated cell, invisible to the naked eye (approx. 40μm) and by now, lacking a nucleus. Over and above this, desquamation in the form of visible clusters of corneocytes (scales) is evidence of a dyskeratinisation phenomenon, typical of inflammatory states (eczema, psoriasis, dandruff…). This terminal phase also involves the gradual transformation of those proteins making up the cornified cell envelope (Loricrin, Involucrin, Periplakin..) becoming rigid due to the formation of a series of inter-chain cross-linking covalent bonds under the action of various Transglutaminases (types 1, 3, or 5). The inter-cellular lipids, generated by the Odland bodies and then arranged in a lamellar phase, are themselves also subjected to profound modification, notably hydrolysis (Ceramidases, Phospholipases..). The Phospholipids thus disappear from the surface of the S.C. The intra-cellular content of the keratinocytes does not escape this intense activity : the component keratins and other proteins (Profilaggrin, Keratohyalin, Loricrin..), undergoing gradual transformation (Profilaggrin, Keratohyalin, Loricrin..) and then degradation, are thought to be at the origin of N.M.F (Natural Moisturizing Factors) such as lactic acid, pyrrolidone carboxylic acid and various amino acids with high water retention capacity. In order to function perfectly every one of these enzyme activities requires the presence of a key element which is free water. This latter (and its various solutions) also circulates from cell to cell via transmembrane proteins, the aquaporins. Besides its importance for the enzyme activities mentioned, water also provides strict control of two major factors: the maintenance of a Calcium gradient in the epidermis and the stratum corneum (S.C.) and that of an acidic pH (no notion of pH without water..), both of which are powerful effectors of keratinocyte multiplication and differentiation. In the case of pH for example, two enzymes responsible for the synthesis of the Ceramides (β-glucocerebrosidase, sphingomyelinase) attain peak activity only at acidic pH (5.6 and 4.5 respectively), their activity being considerably reduced at pH 7. Basically, the slightly acidic pH at the surface of the S.C. (pH 5-6) is due essentially to the constant presence of lactic acid, final « waste product » of the anaerobic metabolism of the epidermis and the result of eccrine perspiration.
Briefly, during the formation of this complex structure and its regulation, water occupies a role so fundamental that : i) its internal flow (from the hydrated dermis towards the surface) must be strictly controlled by the intercellular lipids of the S.C. On the surface this is represented by the T.E.W.L. (Trans Epidermal Water Loss) and ii) it must establish itself a gradient in the epidermis, the water concentration increasing from 40-50% in the living basal layers, to 10%-12% in the S.C. because, ultimate paradox, the relative dryness of the skin surface is also the guarantee of an efficient barrier function and in the end, of its hygiene.
The stratum corneum, fruit of the epidermis
Structure
The S.C. is the stage on which a large number of interdependent players come together. This structure 10-15μm thick (the thickness of cigarette paper) on the forearm, for example, is a remarkable stratification of flattened and cornified cells (thickness approx. 0.5μm, width approx. 40μm), devoid of genetic material: the corneocytes. These latter are held together by strong protein « links », the corneodesmosomes. The solidity of their structure is gradually loosened by a range of protease activities and then destroyed thus completely releasing each corneocyte : this is natural desquamation, a sort of constant sloughing of human skin. We estimate that every day, 4-5 grams of corneocytes are thus imperceptibly eliminated from our body by this desquamative phenomenon. We can already see that this is an important factor of natural elimination of all sorts of contaminants present in the skin and on the surface of these dead cells.
The corneocytes can be seen stacked in layers (15 to 20, or more) surrounded by an intercellular medium rich in lipids (Ceramides, Cholesterol, Cholesterol Sulphate, Triglycerides…), in an organisation often compared with a « bricks and mortar » structure. A picturesque image but which suggests that these inter-cellular lipids (epidermal lipids), represent « adhesive » or inter-corneocyte biochemical mortar. Whilst these lipids do have a true function of controlling water diffusion in the S.C, they are absolutely not responsible for inter-corneocyte adhesion which is the role of specific structures, the corneodesmosomes.
Function
The major function of the S.C.; is that of a barrier. It is in a sense a « dead » structure protecting the living epidermal cells underneath. The table II summarises the main barrier functions exerted in a normal state, unmodified by any skin disorder. It provides an overview of the serious consequences of events (e.g. burns) which cause it to disappear suddenly (dehydration, infection…).
The surface film
The skin surface, like that of our planet, exhibits various « climates » from one skin site to another. This is because the accessory functions (sebaceous, apocrine sweating..), which are not uniformly distributed, make up widely different surface biochemical environments although its acidic pH (from 5 to 6 in general) is the common denominator. The virtual absence of any sebaceous function in the extremities (forearm, legs, feet..) is to a large extent responsible for the increased frequency of xerosis cutis on these sites. Elsewhere, the naturally occlusive nature of the underarms, with copious perspiration and high temperature make a more « tropical » climate. As for the sebum-rich regions (face, back, scalp..), in which lipophilic resident flora flourish, the interactions between this and the host tissue cause inflammatory processes extremely disturbing S.C. physiology (acne, dandruff..). From a practical point of view, cleansing and moisturising products must be made to adapt to these skin climates. Their efficacy may be measured by numerous devices, including the recent Skinchip® which, by contact with thousands of sensors, generates maps of skin surface hydration and its micro-relief [14]. Well hydrated or re-hydrated, the properties of the S.C. to conduct tactile nervous impulses are improved. Lastly, a criterion of consequence, the thickness of the S.C. is found to be highly variable, 15μm to 1mm or more in the case of the palms or soles (in adaptation to their exposure to friction and constant stress). Such thickness is in fact a remarkably effective barrier against various agents including UV radiation.
1.2 - THE DERMIS
Support tissue just under the epidermis, providing the major part of the mechanical properties of the skin, it is however, thicker (1 to 2mm depending on the area) than the latter. In contrast to the epidermis, it is composed rather of a dense network of macromolecules (Collagen, Elastin, Glycosaminoglicans) rather than the cells (fibroblasts) which have synthesised this extra-cellular matrix. Due to its composition macromolecules, the dermis fulfils 3 major functions:
i) reservoir of free and bound water, ii) tissue providing support and physical resistance to mechanical stress (flexibility, firmness) and iii) anchor tissue for the sub-epidermal blood circulation and skin appendages.
With age and exposure to the sun, the dermis undergoes profound transformations : some macromolecules decline in numbers (collagen), hydrolysed by the metalloproteinases (MMPs) in the fibroblasts whereas others reticulate i.e. they thicken and accumulate (Elastose) or are modified by the addition of sugars (Glycation). This produces a dermal tissue which is less flexible, less well hydrated. These events are particularly clear in the superficial part of the dermis (papillary dermis), which is thus less able to provide the epidermis with soluble substances or immune blood cells. Ultra-sound recordings show the gradual appearance in this zone of a non echogenic band (as free water content declines) which thickens with age and exposure to the sun, both of which lead to the appearance of profound modifications such as facial wrinkles on the surface.
1.3 - THE APPENDAGES
Eccrine and apocrine sweat glands
Four major criteria differentiate these two appendices (Table III): i) function, ii) location and anatomy iii) productions and iv) the manner in which they are regulated.
Axillary odours
The underarms are a special micro-ecological environment: relatively occluded, with a higher temperature (approaching 37°C whereas the skin is about 33°C) and high humidity. They also contain large numbers of two types of sweat gland and make up a biochemical medium especially rich in sebum, water, lipoproteins, steroid hormones, salts, amino acids, urea. The production of sweat and the intensity of the odours developed are greater in men than in women (see Male/Female Skin, below) doubtless due to more intense sebaceous activity. It is to be expected that this type of environment would select a specific resident flora particularly rich in bacteria of the genera Staphylococcus and Corynebacterium. The latter produce enzymes which transform this environment, releasing numerous volatile and often malodorous substances to which are added some traces of ammonia generated by the transformation (urease) of the urea into sweat. At the present time it appears clear that these malodorous compounds vary with the individual and constitute differing profiles, composed of trans methylhexenoic acid, 3-hydroxy 3-methylhexanoic acid, certain androstenes, or sulphur compounds such as 3-sulfanylalkan-1-ols-2-5 in various proportions. In short, one single compound cannot sum up the inter-individual variability of axillary odour, by analogy with other substrates (wines, alcohols, vegetables, cheeses, fruits, flowers…) also having subtle and different blends of odours.
Axillary sweat is thus the primary source of the development of such volatile compounds and their prevention or inhibition using topical cosmetics can involve two lines of action, alone or together, besides, of course essential actions of daily hygiene (showering, washing) : i) to prevent or reduce sweating i.e. antiperspirants and/or ii) to slow the development and microbial activity of the axillary flora by antibacterial action. Table IV summarises their principal characteristics.
The sebaceous glands
Producer of sebum (a native mixture of Squalene (approx.15%), Triglycerides (approx. 60%) and Waxes (approx. 25%), the sebaceous glands are not uniformly distributed over the human body. Attached to every hair follicle (terminal as well as vellus hair), they are concentrated in the upper regions (face, scalp, upper chest) where their density approaches 600/cm2, and absent from the terminal regions (hands, feet). The zones rich in Sebaceous Glands are the main sites of Oily Skin and facial acne (the scalp is not involved) and upper back. Over the face itself their density also varies : high on the forehead and central region (nose), forming a T-shaped area called the « T-Zone » which is particularly oily. The relationship between oily skin and diet remains obscure. If there is a link, it is probably more related to the presence of hormone residues (e.g. in milk) than to energy-rich food components (sugars, fats) such as chocolate or cold cuts. This is because from an energy viewpoint, the sebaceous gland is autonomous containing and regulating its own reserves of glycogen.
Depending on the sex (it is a secondary sex gland and highly sensitive to androgens), its production is fairly constant at 0.5 to 2μg/cm2/minute in these areas, but gradually declines after the age of 40 years in virtually all human ethnic groups, becoming inexistent after 70 years. During the ages of maximum sebaceous activity, we estimate that each hour, 50-100 mg of sebum are delivered over the total surface of the face.
2 - SKIN "TYPES"
2.1 - OILY SKIN, DRY SKIN
The opposing pair water/oil is fully expressed in the various skin structures and is the reason why the two substances are preponderant and in variable concentrations in all types of cosmetic formulations.
These two skin types are not mutually exclusive and can co-exist (called a combination skin type) on the face. Whilst Oily Skin is well understood and directly associated with sebaceous function (and its irregular distribution), Dry or rough skin (Ichthyosis vulgaris), is due to an as yet poorly understood process in which the lack of epidermal water/dehydration or cornification is not the only criterion. This latter develops however mainly in the regions of minimal sebaceous function (lower leg, hands, children aged 2 to 11 years in whom sebum is virtually absent). It can however be triggered and/or maintained by external events (dry, intense cold, physical or chemical irritations, exposure to the sun...). Table V outlines the major characteristics of these two skin types.
Oily skin and comedogenesis
Whilst acne is dealt with in another chapter (ibid), it is important to link the syndrome of oily skin to comedogenesis, as Professor A.M Kligman so concisely put it « Sebum fuels the acne flame ». It is thus quite logical that active sebum secretors in particular will suffer from acne. The formation of a blockage in the sebaceous canal (comedogenesis), central feature of the various acneiform lesions, is clearly related to sebum and its modifications, and is nothing to do with the resident flora. In fact when they are formed, 10 % of comedones are found to be sterile. Various hypotheses have been put forward to explain the transformation of sebum into comedogenic substances, such as the peroxidation of squalene, specific component of human sebum present to a level of 12 to 15% and that of other compounds such as free fatty acids. The peroxidation of squalene is also enhanced by UV light, which renders this compound comedogenic, cytotoxic, pro-inflammatory. As expected we find sunlight to have a harmful influence on acne lesions. Furthermore the influence of photo-oxidative substances should be noted, the porphyrins (molecules of similar structure to Haemoglobin or Chlorophyll) secreted by Propionibacteria spp which considerably increase the oxidation of squalene. The synthesis of these pro-oxidative molecules is doubtless linked to the need for micro-aerophilic (or anaerobic) flora to deplete the pilosebaceous duct of oxygen (O2) by fixing it to the 6 double bonds of squalene. When fully oxidised, squalene contains 25% of its weight in oxygen. Moreover, other studies suggest the role of a deficiency in certain anti-oxidants such as certain essential fatty acids, possibly combined with peroxidation phenomena, in the follicles concerned.
In any event, comedogenesis results from the cytotoxic action of oxidised sebaceous compounds on the phenomenon of epidermal keratinisation of the pilosebaceous duct, provoking retention typical of the acne disease. The formation of the comedo « sac », like that of the microcysts now containing flora (bacteria, yeasts), derived from of sebum and cell debris ultimately becomes a truly pro-inflammatory medium. The rupture of such a « sac » will suddenly release this type of milieu into the dermis and is the trigger point of the future inflammatory reaction the major component of which is, this time, clearly under microbial influence. In a way this rupture is strongly analogous to an intra-dermal injection of live micro-organisms and potentially inflammatory compounds of diverse origins (bacterial, fungal, lipid…).
Advice : In fact, comedogenesis initially involves very few follicles of the face or back. This early stage is the moment to prioritise topical treatment with keratolytic or comedolytic compounds from the OTC or cosmetic ranges (AHAs, BHAs, Benzoyl Peroxide, Retinol..) before considering (or avoiding) the use of powerful pharmaceutical agents. Combined with mildly bactericidal cleansing products and sunscreens, their use on retentional lesions is not only effective but reduces the risk of their future transformation into inflammatory lesions. Put simply, comedogenesis is a physiological cutaneous « vicious circle » which needs to be slowed or checked as early as possible.
Table VI summarises the principal factors triggering and promoting comedogenesis.
2.2 - MALE, FEMALE SKIN
At low magnification, structurally and histologically it is impossible to distinguish between male and female skin. However at higher magnification, some structural features slightly differentiate female from male skin. It is however important to note that possible variations are also induced by exposure to the sun, age, care routines etc…From a functional viewpoint, given the differences in hormone balance, there are also a few differences. These latter, both structural and functional are summarised in table VII.
2.3 - SENSITIVE SKIN
Sensitive skin is a common syndrome reported by consumers (mainly women) or professionals. A clear definition is missing however. It is self described as reactive skin and perceived as feelings of discomfort (itching, prickling, burning, pulling…) whereas, no particular symptom is detected clinically. It primarily concerns the face, an area constantly exposed to a variety of conditions (cold, heat, humidity, dryness, wind, sun..). It appears to be extremely variable depending on sex and ethnic group and its physiopathology remains obscure. There appear to be 4 types of inducing (or exacerbating) factors i) intrinsic (age, heredity, hormones..), ii) environmental (cold, sun, pollution..) iii) products (soap, perfumes, cosmetics..) and iv) life-style (diet, alcohol, stress…). A more recent French study conducted on a large number of cases determined the specific « weight » of these various factors related to sensitive skin in the experience of the persons concerned, summarised in table VIII in decreasing order of value. Whilst some of these criteria can be explained from a mechanistic point of view (Cold/Temperature, Soap/alkalis released, Swimming pool/Chlorine, Sun,...), the logic of others remains obscure. It is for instance surprising to find the impact of pollution to be judged the least important.
Testing to determine the severity of sensitive skin is most often conducted by the application, on the wings of the nose, of non toxic but irritative substances such as 10% lactic acid or capsaicin (from 10-5 to 10-3 %), major component of certain spices such as chilli powder. An analogue scale used to record the subject’s sensations during the hour following the application gives a diagnosis of this sensitive skin and its severity. In any case these sensations are transmitted by the C nerve fibres (unmyelinated) of the skin.
Advice/Possible solutions
Cosmetics intended for this particularly complex skin type, involving so many components, are formulated on the basis of several criteria:
– Certain products are formulated « No X, X-free », where X could be various compounds (parabens or preservatives in general, fragrances, alcohol, potentially irritating peeling agents…) suspected of exacerbating or challenging a sensitive and reactive skin. Whilst such an approach is eminently sensible, it does not however resolve the problems of such a skin, as much with respect to causal factors as to its amplitude or severity.
– Inasmuch that such sensitivity may be related to the conjunction of various factors and/or ingredients, the formulations intended for this skin type are particularly restricted, having a minimum number of ingredients, selected from experience as being perfectly well tolerated for decades, like products intended for children.
– When buying and using a new product people with sensitive skin are therefore advised to apply it with gradually increasing frequency (once a week, then twice a week…) in order to ensure that it feels suitable for them.
3 - HYGIENE AND SKIN MOISTURISATION
3.1 - THE PARADOXE OF THE S.C.: DRY ON THE SURFACE, HYDRATED INSIDE
Besides the presence of sweat and sebaceous film, the skin surface made up of the terminal corneocytes of the Stratum Disjonctum is naturally dry and hydrophobic, a truly impervious barrier. Under conditions of prolonged exposure to a humid environment (>80%), or even immersion in water, the barrier function of the S.C. decreases but will, in contrast increase sharply under dry environmental conditions (<20%). It is accepted that 40-60% relative humidity (RH%) is an optimal condition for the function of the S.C. It is for this reason that the use of occlusive systems, while necessary, must be as short as possible. Occlusion, often used therapeutically in the form of patches to enhance the penetration of active substances (Trinitrin, Nicotine, Oestrogens..) is hardly a problem when restricted to small surfaces (a few cm2). But when applied to larger areas, this can provoke a longer-term serious « micro-ecological » change in the skin microbiome. Water accumulates on surface, the pH increases and the resident flora (see below) rapidly changes, promoting the development of a transient, potentially pathogenic flora. It was for this reason that during the Vietnam War (1962-1975), a considerable number of GIs suffered from « athlete’s foot », i.e. fungal infections of feet almost constantly wet, occluded in tight boots, in a tropical climate. In case of a minor skin wound, a prompt as possible return to a dry S.C. is doubtless the best guarantee of a rapid restoration of its protective structure. In contrast, the development of xerosis cutis (occasional or constitutive) leading to a disorganised, disrupted S.C. facilitates the penetration of external elements likely to amplify or provoke unpleasant sensations (pruritus…).
3.2 - THE SURFACE OF THE S.C. AND ITS VARIOUS CLIMATES: SKIN OR SKINS?
The skin surface, like that of our planet, exhibits various « climates » from one skin site to another. As the appendages (sebaceous glands, apocrine sweat glands..) are unevenly distributed, highly different biochemical environments are formed on the surface. The near absence of sebaceous function on the extremities (forearms, legs, feet..) is the main explanation of the increased frequency of xerosis cutis on these sites. Elsewhere, the naturally occlusive character of the underarms, with high levels of sweat and high temperature is a rather « tropical » climate. In the case of sebum-rich regions (face, back, scalp..), which encourage the development of a lipophilic resident flora, the interactions between this and the host tissue are the origin of inflammatory processes highly disturbing for the physiology of the S.C. (acne, dandruff..). Lastly, a criterion of consequence, the thickness of the S.C. is found to be highly variable 15μm to 1mm or more in the case of the palms or soles (in adaptation to their exposure to friction and constant stress). Such thickness is in fact a remarkably effective barrier against various agents including UV radiation.
3.3 - THE S.C. SURFACE, MICROBIOL NICHE, PIVOTAL FOR HYGIENE
Resident flora
The skin surface is anything but sterile. The various media of the surface of the S.C. represent diverse « microbiota » which, by strict Darwinian adaptation, select the microbial species capable of developing there, the resident flora, mainly Gram+. These become established soon after birth and are found to be relatively stable both qualitatively and quantitatively, over a lifetime. The density of colonisation on the surface, depending on the site, is extremely variable, i.e. 102/cm2 to 107/cm2 and the oily regions (face, back, scalp) are home to a particularly lipophilic flora (Propionibacteria, Malassezia, Staphylococci..). Sebum and derivatives are their primary food source, broken down by their enzyme systems (Lipases, oxidases..) releasing Glycerol, moisturising agent of the S.C. par excellence (see below). Dry areas (lower leg..), where the rarity of free water is by definition hostile to microbial development, are not surprisingly, sites of low colonisation.
Transient flora
Transient flora (essentially Gram -) brought by simple contact or by the air is found at low levels of colonisation. It generally survives only a short time, the dry surface of the S.C. being hostile to their development and rapidly destroyed under the action of epidermal biocides (defensins) or bacteriostatic peptides synthesized by the resident flora (Epidermin, Gallidermin). Staphylococcus aureus survives only a few hours on the surface of a S.C. in good structural condition. However the least « portal of entry » (cut, burn..), by disruption of the S.C., can be the initial source of a skin infection, these strains finding the best medium for their survival and colonisation. Experimental attempts to trigger infection have clearly shown that this is impossible on healthy S.C.
Taken together, a sort of « micro-ecological » balance of the skin is at the centre of the mechanisms of propagation of uncountable nosocomial diseases. It has been shown that the increase in the frequency of simple hand washing (or application of antibacterial gels) leads to a clear decrease in the prevalence of infections in a hospital setting.
These microbiological concerns appear to be at the heart of the hygiene-hydration duality : a properly hydrated S.C., i.e. perfectly organised, represents the very first line of defence against disease.
3.4 - PRATICAL ADVICE
Cleanse, hydrate, protect
Very early on Ancient Greece, as did Rome later, associated water (public baths, spas) with hygiene, from the name of the Greek Goddess « Hygeia », health and cleanliness. Water, source of life, crucial biologically, takes on another dimension : it becomes the symbol of the purifying agent, maintenance of a healthy lifestyle in the individual sense. In this more recent version it becomes the indispensable ally of cleanliness and disinfection of the skin, a covering at the frontiers of the organism and of an external world full of « transmissible visitors » or all sorts of ill timed agents. Water, now becomes the source of « social » hygiene. To this is added of course, compounds of all origins, including soap, various essences and hydrating compounds with, finally, the famous surfactants, highly safe and effective in use. To summarise, water and the skin, their intimate relationships converge : well hydrated, the skin becomes a hygienic tissue. In return, perfectly cleansed on its surface, rid of potential aggressors, it can fully take on its physiology of natural hydration.
Water alone, of course, is not sufficient to guarantee good skin hygiene. This latter, in keeping with its definition, aims to fulfil four complementary objectives : cleansing, disinfection, maintenance and structural non aggression. To non detersive water, soap was the « ancestral » adjuvant, formed by saponification of vegetable oils with strong bases (Sodium, Potassium hydroxides) the foam, an airy emulsion eliminates all sorts of contaminants. Due to its structure however (« soap effect »), it has a tendency to become dissociated on the skin during washing, partially releasing the strong bases, the cause of irritation due to the sudden (but temporary) increase in skin pH to as high as 9-10. The 1950s saw the development of new non- or very slightly dissociable agents, amphiphilic in nature, the Surfactants. Their intense development since then along with constant innovation have enlarged their diversity and type (anionic, cationic, non ionic, amphoteric..) and provided a perfect balance between safety and efficacy in use. Rarely used alone, but blended according to the target skin sites, they provide rapid and effective hygienic action and are available in uncountable forms (dermatological syndet bars, shampoos, shower gels etc..). Their characteristics, safety, modes of action, structure.. have been widely reported in the literature and excellent syntheses of this are to be found in various articles.
Whilst water is an essential vehicle, it is absolutely not a skin moisturiser, the S.C. surface being particularly hydrophobic. The « wetting » of this, made possible by surfactants (cleansing products, care creams, make up removers etc..), provides thus the addition/supply of hydrating components including the famous and ubiquitous Glycerol, ensuring complete safety and great efficacy, in complement to the N.M.F., alpha or beta-hydroxy-acids, urea, etc.. These various components do not provide water but, by inserting themselves in the structures of the S.C. (cells and inter-cellular spaces), they fix free water and/or slow down surface evaporation : the S.C. is thus property hydrated to an extent which is modified by varying concentrations and appropriate to the specific sites (oily, dry). Also modified according to the need to accompany excessively drying events or therapies (xerosis cutis, after sunburn, retinoic acids (all trans or 13-cis). Another strategy of maintenance of hydration of the S.C. in states of xerosis cutis, other than active moisturisers, consists of applying slightly occlusive formulae which due to their thick, oily, film-forming nature, very often based on petroleum jelly, form a sort of « screen » greatly slowing trans epidermal water loss (T.E.W.L.) and restoring the integrity of the S.C. Finally, skin ageing, chronological or photo-induced, by thinning of the S.C. leads to xerosis cutis, the manifestations of which, clinical and also sensory, are considerably relieved and prevented by the regular use of emollient and moisturizing formulae the contribution of which to skin comfort is not the least benefit. The last paragraph gives examples of the major types of formulations possible which provide daily care, sun protection, hygiene, anti-ageing etc.
Sun protection is mandatory
The effects of the sun, more particularly its UV B (290-320nm) and A (320-400nm) radiation, are the subject of an abundant literature the conclusions of which concord in the immense majority. While low doses of this radiation possesses some positive properties (Vitamin D synthesis, endorphin release..), at high doses it has serious consequences for the skin in the short, moderate and long term. These depend on the doses received (duration of exposure multiplied by radiance) and will not have the same magnitude depending on the Photo-types concerned.
Sun protection is thus mandatory and must comply with 6 fundamental points:
1) Make children a priority. It is nowadays well established that the most severe long term consequences arise from acute exposure of the skin to the sun when young. Two basic rules: a) no exposure to the sun for infants (« baby » phase) and b) at the age when children become independent (walk, run, play outside), adopt the Australian rule of « Slip, Slap, Slop », i.e. slip on a T-Shirt, slap on a hat/cap and slop on generous quantities of sunscreen to the exposed part of the body (face, hands, legs, arms and forearms…).
2) No protection B if not balanced with protection A. The current rule suggested and adopted in Europe is that of a third. The protection factor A (PFA) must be equal to at least one third of the B protection (SPF). A product with an of SPF30 should thus also have a PFA ≥10.
3) Be adapted to daily life. The sunscreen for a farmer or a fisherman obviously needs to be more powerful than one for someone working in an office every day.
4) Be adapted to Photo-type. Pale white skin types (Photo-types I-II) need a high sun protection factor. These subjects are known to be the most likely to develop melanoma in the long term. The same is true for persons tending to develop photo-allergic phenomena such as lucitis (mainly UVA) or who are subject to various dermatoses (acne, rosacea, melasma…).
5) Be adapted to summer conditions. UV radiance varies with altitude (high in mountainous regions), latitude (high at the equator), time of day (high at the zenith), ground reflection (snow, sand, water…) and of course, duration and frequency of exposure.
6) Be applied as recommended. The factors mentioned above (SPF, PFA) on the packaging of sunscreens are obtained - and validated - under standard conditions, notably the quantity of product applied (2mg/cm2). Under real-use conditions, consumers actually apply 2 to 3 times less (0.6-1mg/cm2). This results in lower solar protection and frequent re-applications are necessary, depending on the sunlight, as indicated on all products.
NB : It is important to mention that « tanning » without UV light, using artificial coloration of the S.C. (Dihydroxyacetone, DHA, products called sunless tanners) do not provide any significant UV protection. Similarly, tanning in UVA tanning booths must be closely monitored and regulated.
For children’s skin
Contrary to widespread belief, the skin of a full-term baby is perfectly functional with respect to its main purposes, unlike that of premature infants. However, pigments and immune functions (Langerhans cells) are still fragile and respond poorly (few effectors) to photo or immune stress, which justifies the last point mentioned above.
Apart from the above, the skin of children aged 3 to 11 years (pre puberty) hardly exhibits any notable symptoms apart from a tendency to slightly dry skin (xerosis cutis), related to the near absence of sebum. This is effectively relieved with simple moisturisers.
« Baby » products (cleansers, moisturisers) comply with two strict rules: i) they contain as few ingredients as possible and ii) are selected for their well known and excellent safety. For washing the body of a baby « syndet » based products should be favoured rather than soaps, likely to temporarily release traces of strong bases (Sodium, Potassium hydroxides).
Make-up
The use of make-up was probably one of the first decorative activities of prehistoric man and later, the Egyptians. Besides its decorative function, make-up is a precious ally of skin care and aesthetic comfort. It can, for many people, camouflage certain unwanted features of ones own image. The immense palette of shades available on the market offers an adaptation to each skin colour combined with the utmost discretion. Current formulae, light, liquid, non occlusive, are not only easy to apply but also contribute to the maintenance of good moisturisation of the S.C. Certain specialised products such as lipstick also moisturise, the lips being prone to dehydration. They are easily removed in the evening using effective and moisturising make-up remover emulsions. The presence of mineral pigments in the formulae may give some products slight photoprotection. The daily use of make-up does not, contrary to popular belief, exacerbate a disorder like acne or provoke it. The use of make-up is not only compatible with certain dermatological treatments (including acne) but provides additional benefit of well-being (self esteem) in many cases where facial beauty/appearance is compromised (acne, dyschromia, vitiligo, scarring, rosacea, melasma…), or simply disguise the shiny appearance of an oily skin.
3.5 - THE DIVERSE FORMULATIONS (AND INGREDIENTS) OF CARE, HYGIENE AND PROTECTION PRODUCTS
These products are immensely varied in texture and highly variable in the composition of their hydrophile-lipophile balance, a reflection of the organisation of the epidermis and the Stratum Corneum. This diversity delivers an effect and also fulfils the desire for pleasure or comfort depending on skin type or personal preference. Figure below illustrates the various principles of formulation, ranging from a total water phase to a total oily phase. Their gradual blending via the emulsification process, gives an infinite range of products. The figure summarises the properties of the majority of formulations, their appearance and how they are appropriate for certain specialised applications. Less common formulations (sticks, sprays) are not described as they are not used daily, although they are highly effective.
3.6 - SAFETY AND POTENTIAL ADVERSE EFFECTS
Under normal conditions of use, these products are very well tolerated and have been tested to show this before marketing. Constant post-marketing surveillance for adverse effects of cosmetics (used by millions or billions of consumers) reveals minor adverse effects (irritation, dry skin, various forms of discomfort) in the order of 5 to 50 (depending on the product) for 10 million units sold, in a « normal », population i.e. free from any particular skin sensitivity. Qualitative analysis of this data reveals the following frequent causes, non exhaustive:
– Misuse or inappropriate choice for the principal use of the product: product for the body applied to the face or a hydro-alcoholic gel on dry skin.
– Application of incompatible products on top of each other: lotion and oily gel for example. This makes it difficult to find the « culprit».
– Use of a product on a previously disturbed (sunburn, intense scrub...) or broken skin (slight cut, graze..).
– Interference of the products with a keratolytic, peeling dermatological treatment which also leads to greater sensitivity to sun exposure.
The major problem encountered remains of course the allergic (or Photo-allergic) type phenomenon which is much higher in subjects with constitutionally sensitive immune system. This allergic reaction (contact dermatitis), due to a single ingredient, can produce severe symptoms. Whilst such a reaction is not limited to cosmetic ingredients (cf. Nickel/Jewellery, food/peanuts/shellfish, antibiotics…) in most cases they involve preservatives or fragrances and are the reason for their gradual elimination and, as is to be expected, numerous formulae free from preservatives or fragrances are now available. The identification of the « guilty » ingredient with dermatological tests and follow-up to the product labelling (Full Ingredient Labelling, see Table IX: technical note on F.I.L.) is possible, effective and recommended for these subjects. Nevertheless, practical advice to this sensitive population is : test any new product before its regular use, by a small dab (behind the ear or in the elbow fold). If no particular symptom has appeared within 24-48 hours, (redness, œdema, peeling, local pain..), the product will be tolerated. It is the same approach (« spot test ») as must be recommended by all manufacturers to persons using hair dyes.
×
N.B. : This limited content is for the general public. If you are a health professional, click here to register for free and gain access to a dedicated deeper content.
If you already have an account, log in!
Therapeutics in Dermatology, Fondation René Touraine © 2001-2015








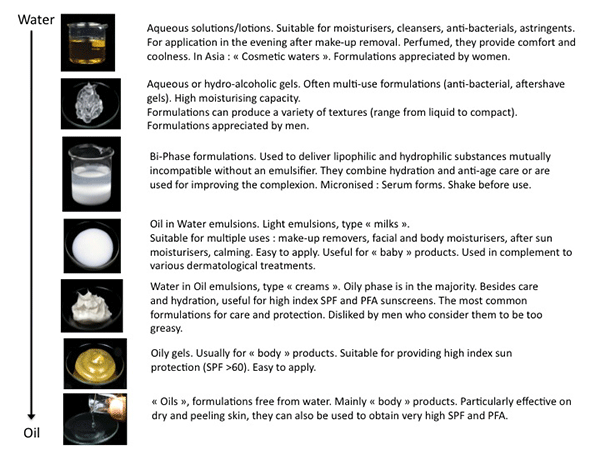 Figure:
Figure: 






